Bowel cancer is one of the most common and preventable cancers in many countries. Knowing the main risks, spotting early warning signs, and making healthy choices can help lower your chances of getting bowel cancer. Understanding the basics now can make a big difference for your future health and peace of mind.
Many people do not notice bowel cancer early because the signs can be small or easy to miss. Getting regular screening tests is important because it can find problems before they turn serious. Simple changes, like eating more fiber and staying active, can also help you avoid this disease.
Key Takeaways
- Early detection and healthy habits reduce bowel cancer risk
- Knowing the main symptoms and risk factors is important
- Regular screening keeps you safer over time
Understanding Bowel Cancer
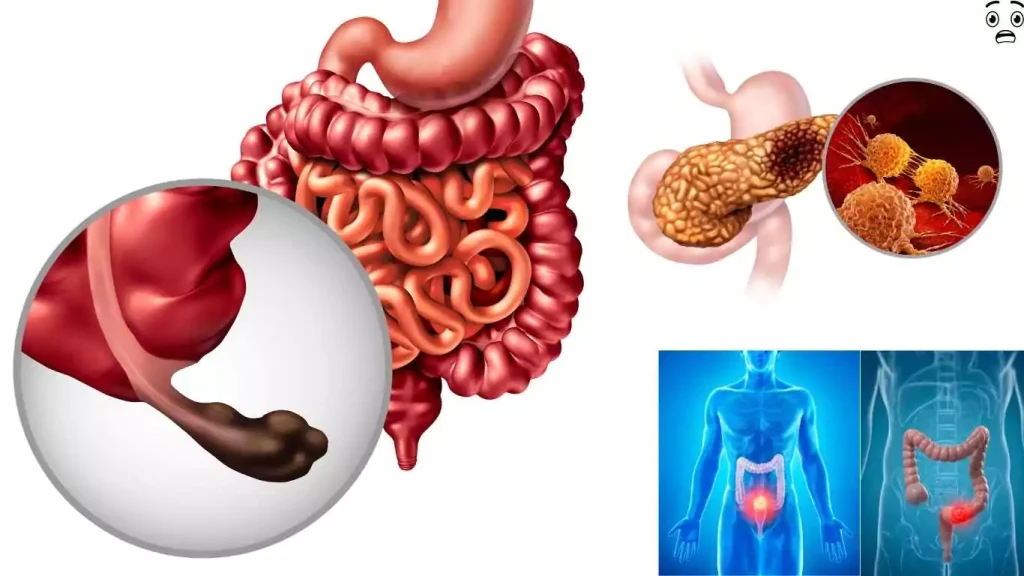
Bowel cancer, also called colorectal cancer, can develop in different parts of the large intestine. Knowing how this cancer starts, the common types, and the way it develops helps people spot warning signs early and know their risks.
What Is Bowel Cancer?
Bowel cancer is a disease that begins in the cells of the large intestine. This cancer most often affects the colon or rectum. It is known medically as colorectal cancer. Most cases start as small growths called polyps, which can slowly turn cancerous over time.
People over 50 are at higher risk, but it can happen to younger adults, too. Family history, certain genetic conditions, and lifestyle habits like high red meat intake also increase risk. Common early symptoms include changes in bowel habits, blood in stool, or unexplained weight loss. Early detection improves treatment outcomes. For more details on signs, risk factors, and screening, visit this colorectal cancer information page.
Types of Bowel Cancer
There are several types of bowel cancer, but most start in the lining of the bowel. The most common type is adenocarcinoma, which makes up over 90% of cases. This type begins in the glandular cells that line the bowel wall.
Other rare types include carcinoid tumors, lymphomas, and sarcomas. Carcinoid tumors begin in hormone-producing cells. Lymphomas start in immune system cells. Sarcomas start in the muscle layers or blood vessels of the bowel. Treatment and outlook depend on the type and stage of the cancer at diagnosis. To learn more about the types and causes, check out this bowel cancer overview.
How Bowel Cancer Develops
Bowel cancer often develops slowly over several years. Most cancers begin as polyps — small, non-cancerous growths in the inner lining of the colon or rectum. Not all polyps turn into cancer, but some can change over time in a process called dysplasia.
As abnormal cells gather, the polyp may become cancerous and grow into the bowel wall. If not detected or treated, cancer can spread to nearby tissues and even other organs, especially the liver. Early prevention and regular screening can detect polyps before they turn cancerous. For more on how bowel cancer forms and spreads, visit this bowel cancer information page.
Causes and Risk Factors
Bowel cancer develops due to a combination of inherited genes, lifestyle habits, and exposures in daily life. Some risks can be lowered, while others cannot be changed.
Genetic Predisposition
A family history of bowel cancer can raise a person’s chances of getting this disease. Certain inherited conditions like Lynch syndrome and familial adenomatous polyposis (FAP) are linked to a higher risk. These gene changes can be passed from parents to children, making early screening and regular checkups important for families affected by these syndromes.
Age is another strong factor. The risk rises quickly after the age of 50. Gender also plays a role, as men are slightly more likely to develop bowel cancer than women. Genetic risks are not influenced by lifestyle or environment. Those with first-degree relatives affected by bowel cancer should talk to a doctor about testing and prevention.
Lifestyle-Related Risks
Eating habits play a large part in bowel cancer risk. High red meat or processed meat intake, low fiber diets, and heavy alcohol use may increase the chances of developing the disease. Being overweight, lack of exercise, and smoking are also well-known risks linked to bowel cancer.
Common lifestyle risks include:
- Eating a diet high in red or processed meats
- Not eating enough fruits, vegetables, and fiber
- Drinking alcohol regularly or in large amounts
- Smoking tobacco products
- Being overweight or obese
- Getting little or no physical activity
Improving diet, being active, and stopping smoking can lower these risks. Making changes in daily habits can have a meaningful impact on preventing this cancer.
Environmental Factors
Long-term exposure to harmful chemicals or working environments can play a role in bowel cancer. Some studies suggest that people who work with certain industrial chemicals may have a slightly increased risk, but this link is not as strong as that with lifestyle or genetic factors.
Living in places with poor air quality or high pollution has not been clearly tied to bowel cancer, but ongoing research continues in this area. Use of certain medications, such as long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs), may actually lower the risk for some people. However, taking these drugs carries other health risks and should only be done on a doctor’s advice.
For most people, environment plays a smaller role compared to inherited and lifestyle-related risks, but it is still important to consider overall health and workplace safety. More on these environmental influences can be found at Cancer Research UK.
Recognizing Symptoms Early
Bowel cancer can start with mild symptoms, but noticing changes early makes a big difference. Knowing what to watch out for and when to talk to a healthcare provider can help people get the care they need sooner.
Common Warning Signs
Some warning signs of bowel cancer can show up early, even if they seem mild at first. One of the most common is a change in bathroom habits, like diarrhea or constipation that lasts for several weeks. Noticing blood in the stool, which may look bright red or very dark, is another sign that should not be ignored.
Other possible symptoms include unexplained weight loss, feeling very tired all the time, or stomach pain that does not go away. People may also notice their stool looks thinner than usual. Sometimes there is a sense that the bowel does not empty fully.
Keep in mind, these symptoms can be caused by other conditions too. However, if they appear suddenly or do not improve, they could point to a more serious issue like bowel cancer. To read more about early signs and what to look for, see this list of early warning signs of bowel cancer.
When to Seek Medical Advice
It is important for people to contact a healthcare provider if these symptoms last longer than a few weeks or get worse over time. Blood in the stool, ongoing stomach pain, and sudden weight loss should be checked out by a doctor quickly, even if these signs do not seem severe.
People with a family history of bowel cancer or other risk factors should be even more careful. Regular screening can help find problems before they become serious. Doctors can suggest the right tests based on personal risk and symptoms.
For more in-depth details about when to call a doctor and what symptoms matter most, review the advice about when to seek medical help for colorectal cancer symptoms. Early guidance from a healthcare professional offers the best chance for a good outcome.
Diagnosis and Screening Methods
Doctors use several ways to find and check for bowel cancer. Finding the disease early can greatly improve treatment success and help prevent serious health problems. Screening tests and diagnostic procedures are key to spotting bowel cancer at its earliest, most treatable stages.
Screening Recommendations
Many experts recommend starting regular bowel cancer screening at age 45 for people with an average risk. Some may need to start earlier if they have a family history or other risk factors.
The most common and reliable test is a colonoscopy. This procedure is usually done every 10 years if results are normal. Other screening tests include stool-based methods like the FIT (Fecal Immunochemical Test), stool DNA tests, and the guaiac-based fecal occult blood test (gFOBT). These stool tests look for hidden blood or abnormal DNA in a person’s stool and may be needed each year or every three years, depending on the specific test.
Visual tests such as the flexible sigmoidoscopy and CT colonography (virtual colonoscopy) are also options, though less common than colonoscopy. Doctors help patients choose a test based on their health, risks, and preferences. Read more about the different colorectal cancer screening options.
Diagnostic Procedures
If a screening test shows something unusual, doctors will usually order more tests to find out if cancer is present. The most direct way to examine the colon is a colonoscopy. This involves guiding a flexible tube with a camera into the colon to look for polyps or growths. If a polyp or tumor is found, the doctor may remove a small piece to test in a lab. This is called a biopsy.
Doctors might also use imaging tests such as CT scans, MRI scans, or ultrasounds to see if the cancer has spread to other parts of the body. Sometimes, blood tests are used to check for substances made by tumors. Each of these procedures helps build a clearer picture of the patient’s health so doctors can plan the best treatment.
Importance of Early Detection
Early detection of bowel cancer can save lives. Tumors found in their earliest stages are much easier to treat, and the chances for a cure are much higher. People who do regular screening often find problems before cancer causes symptoms.
Screening can also find precancerous polyps. Removing these polyps can stop them from turning into cancer. This means that screening not only helps find cancer but can actually help prevent it from starting.
For people with higher risk, such as those with a family history, screening may start before age 45 and may happen more often. Following recommended screening guidelines is one of the best ways to lower the risk of serious illness. For more on spotting colon cancer without a colonoscopy, visit this detailed guide.
Prevention Strategies and Lifestyle Changes
Certain daily habits can make a difference in lowering the risk of bowel cancer. Eating well, staying active, and avoiding alcohol and tobacco are proven to help protect against this disease.
Healthy Diet Choices
A diet high in vegetables, fruits, and whole grains can reduce the risk of bowel cancer. Foods high in fiber, such as beans, lentils, and brown rice, help digestion and keep the colon healthy. Reducing red and processed meats, like bacon and sausage, is linked with a lower risk.
Choosing foods with vitamins, especially vitamin D and calcium, can also be helpful. Limiting sugary snacks and processed foods can help manage weight and lower the chances of getting bowel cancer. Drinking plenty of water supports bowel health.
The American Cancer Society notes that eating less fat, especially from animal sources, and adding more plant-based foods makes a difference. For more details on how diet changes affect risk, read about colorectal cancer prevention and healthy eating.
Regular Physical Activity
Regular exercise plays a key part in lowering bowel cancer risk. Even simple activities like walking, gardening, or cycling can be helpful. Aim for at least 30 minutes of moderate exercise most days of the week.
Physical activity helps maintain a healthy body weight, which lowers the risk of not only bowel cancer but other health problems too. It also helps the digestive system work better and can lower inflammation in the body.
Small changes, like taking stairs instead of the elevator or walking short distances, add up over time. Those who are more active tend to have a lower risk, according to research from Baylor Medicine.
Reducing Alcohol and Tobacco
Drinking less alcohol and not smoking are important ways to prevent bowel cancer. Alcohol has been shown to increase the risk, especially with heavy or regular use. It is best to drink only small amounts or avoid alcohol completely.
Smoking also increases bowel cancer risk. Quitting smoking at any age brings health benefits and can help the body repair itself over time. Both alcohol and tobacco often increase inflammation and can harm digestive organs.
Limiting these habits not only lowers the risk of cancer but also benefits heart, lung, and overall health. For more information about cutting alcohol and quitting smoking, the Mayo Clinic Health System explains safe steps and further prevention methods.
Long-Term Management and Support
Long-term care is important for people who have been treated for bowel cancer. Regular doctor visits help check for signs of the cancer coming back and watch for late side effects of treatment. Most doctors suggest follow-up appointments every few months for the first couple of years.
Some survivors may face lasting health issues, such as digestion problems or changes in energy. Making healthy lifestyle choices—like eating balanced meals and staying active—can help manage these effects.
Support from others is also key. Many people benefit from joining support groups or talking to a counselor. Family and friends play an important role, and open communication helps many survivors feel better about their bodies after treatment. You can find more about these approaches through the American Cancer Society’s guide.
Monitoring for new or ongoing problems is common, since bowel cancer can require chronic care. Recurrence and late effects should be addressed quickly. Ongoing checkups give peace of mind and help catch any issues early. Read more about long-term care routines at allseniors.org.
Tips for Bowel Cancer Survivors:
- Keep all follow-up appointments
- Share concerns with your healthcare team
- Find support groups or counseling
- Prioritize nutrition and exercise
| Key Focus | Examples |
|---|---|
| Medical Monitoring | Regular checkups, scans |
| Emotional Support | Counseling, support groups |
| Healthy Habits | Diet, physical activity |
Frequently Asked Questions
Screening can catch colorectal cancer early, which improves treatment results. Recognizing signs and using tests like the FIT kit or a colonoscopy plays a big role in prevention and early detection.
What are the recommended guidelines for colorectal cancer screening in Singapore?
In Singapore, adults with average risk should start regular screening at age 50. For those with a family history of the disease or other risk factors, screening may begin earlier. The two most common screening options are the Faecal Immunochemical Test (FIT) yearly, or a colonoscopy every 10 years. More info is available from colorectal cancer screening recommendations.
How can one check for signs of colon cancer?
Doctors use different tests to check for colon cancer. The most common first step is a stool test such as the FIT, which looks for hidden blood. If the result is positive, a colonoscopy is recommended to look inside the colon for polyps or cancer. Self-checking at home is not effective, so regular tests are needed.
What are the common symptoms associated with colorectal cancer?
Colorectal cancer often causes changes in bowel habits, like diarrhea or constipation. Blood in the stool, abdominal pain, unexplained weight loss, tiredness, and feeling that your bowels don’t empty completely are also common symptoms. Many of these may be caused by other problems, so it is important to consult a doctor if these occur.
At what age should one start getting screened for colorectal cancer?
Most healthy adults should start screening at age 50. However, those with higher risks, like a family history of colon cancer, may need to start earlier. Doctors may adjust timing based on personal and family medical history. Details on when to start screenings are on colorectal cancer screening questions.
What is a FIT test kit and how does it aid in detecting colon cancer?
A FIT test kit is a simple stool test that checks for hidden blood, which can be an early sign of colon cancer. It does not require diet changes and can be done at home. If results are positive, further tests like a colonoscopy may be needed. Learn more about the FIT test kit.
How much does a colonoscopy screening typically cost in Singapore?
Colonoscopy costs in Singapore vary depending on the clinic and whether it is done in a public or private hospital. The price usually ranges from about S$800 to S$2,000 before government subsidies or insurance. Patients are encouraged to check with healthcare providers about costs and financial assistance options.